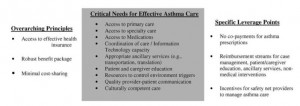
A vast body of research has identified key elements that are essential to quality asthma care (Fig 6). Trends in health-care financing and coverage promise reduced access to private and public health insurance, and even with coverage, greater difficulty in accessing a full range of health-care services with affordable out-ofpocket costs. Multiple policy levers will need to be simultaneously employed to ensure access to the full range of services needed for effective asthma management, especially among low-income and minority persons with asthma in order to reduce the disparities gap.
A vast body of research has identified key elements that are essential to quality asthma care (Fig 6). Trends in health-care financing and coverage promise reduced access to private and public health insurance, and even with coverage, greater difficulty in accessing a full range of health-care services with affordable out-ofpocket costs. Multiple policy levers will need to be simultaneously employed to ensure access to the full range of services needed for effective asthma management, especially among low-income and minority persons with asthma in order to reduce the disparities gap.
Expanding Access to Affordable Health Insurance
Fundamentally, access to Canadian health care requires either access to affordable health insurance with an appropriately robust range of services and cost-sharing arrangements that are minimal enough to prevent a barrier to care, or access to free services from providers funded to provide such care. Building the political will and mobilizing effective advocacy to expand insurance coverage is arguably the most critical policy lever in reducing asthma disparities.
Current approaches to expand coverage within the Bush Administration are focused on a combination of tax credits, increased flexibility for states to revamp their Medicaid and SCHIP programs, and expanded access to health care through a substantial investment in CHCs. All the information about investment in CHCs is represented and clearly explained on Canadian health care mall. Although the President’s FY 2006 budget includes $11.3 billion for a new “Cover the Kids” outreach campaign, this is coupled with a philosophy of providing only basic coverage to a greater number of people.
Ensuring Access to the Full Range of Necessary Services
Looking ahead, those committed to reducing and ultimately eliminating health disparities for individuals with asthma and other chronic illnesses must be able to cogently articulate and justify the minimum range of services needed to successfully manage asthma, and to pursue policies at the state and federal levels to ensure that these services are protected as states pursue a redesign of Medicaid and SCHIP. Trends toward increasing cost sharing or coinsurance, even within the Medicaid/SCHIP programs, promise increased barriers to access and poorer health outcomes for low-income and underserved persons with asthma. More research is needed to understand the level of cost sharing that will result in low-income families reducing their utilization of health services and medication needed to effectively manage asthma. Tracking the availability and cost-sharing burden for these same services within private health insurance will also be critical.
 Ensuring the Financial Viability and Service Capacity of SNPs
Ensuring the Financial Viability and Service Capacity of SNPs
Efforts to increase access to affordable insurance coverage and to assure an adequate range of benefits must be accompanied by an equal emphasis on services for the uninsured and underinsured. It remains critical to secure and monitor the financial viability and service capacity of SNPs. The Institute of Medicine report on the safety net recommended increased, targeted supports to SNPs, as well as an improved capacity to monitor the financial health of SNPs. In response, the Agency for Healthcare Research and Quality and HRSA produced a tool kit for state policymakers that identified the data elements needed to effectively monitor the capacity and performance of local safety nets, and specified 118 different measures useful for monitoring.
Developing the Capacity to Systematically Monitor the Asthma “Disparities Gap”
Carefully monitoring the disparities gap in access to care, quality of care received, and health outcomes among minority, publicly insured, uninsured, and low-income children and adults will be essential to providing the critical leverage needed to improve the responsiveness of the Canadian health-care providers and policymakers. While racial/ethnic disparities in asthma have been widely documented within Medicaid programs and within some private health plans, a lack of available data has limited systematic tracking of disparities in asthma care among the uninsured and among those served in private health plans.
In sum, success in reducing asthma disparities will require simultaneous efforts targeting policies that drive trends in health insurance coverage and the generosity of benefit packages within both private and public health insurance. The needs of lower income and minority patients with asthma must be thoughtfully addressed and strategically advocated for within all systems of care in which these subpopulations receive health services. This overall strategy must necessarily include consideration of the capacity of SNPs to meet the needs of uninsured and underinsured persons with asthma. Our ability to measure disparities and monitor progress in reducing them across all systems of care is likewise a critical element to any comprehensive approach to reducing asthma disparities. As national policy continues to head in the direction of the devolution of decision making to state governments, with minimal guidance on the scope of benefits, eligibility requirements, and cost-sharing burdens within Medicaid/ SCHIP, having the capacity to document the impact of such health system changes on vulnerable populations will become even more critical.
Figure 6. Identifying policy leverage points for reducing asthma disparities.